Treatment
Spinal Injections
When your back or neck problem is severe enough and has not responded to conservative measures, your doctor may recommend a spinal injection.
Spinal injections are used in two ways.
- They can be performed to diagnose the source of back, leg, neck, or arm pain (diagnostic).
- They can be used as a treatment to relieve pain (therapeutic).
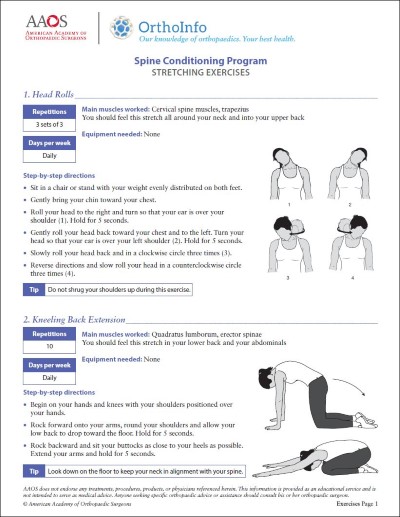
Most spinal injections are performed as one part of a more comprehensive treatment program. Simultaneous treatment nearly always includes an exercise program to improve or maintain spinal mobility (stretching exercises) and stability (strengthening exercises).
Procedure
Spinal injections are performed under X-ray guidance, called fluoroscopy, to confirm correct placement of the medication and improve safety.
To do this:
- A liquid contrast (dye) is injected before the medication.
- If this contrast does not flow in the correct location, the needle is repositioned, and additional dye is injected until the correct flow is obtained.
- The medication is not injected until the correct contrast flow pattern is achieved.
Types of Spinal Injections
Epidural Injection
Epidural injections are used to treat pain that starts in the spine and radiates to an arm or leg. Arm or leg pain often occurs when a nerve is inflamed or compressed (pinched nerve). These injections can also be used to diagnose the source of pain.
- Therapeutic epidural spinal injections involve injecting an anesthetic and/or an anti-inflammatory medication, such as a steroid (cortisone), near the affected nerve. The needle is placed into the epidural space, which is located just outside of the membrane that protects the spinal cord. The medication reduces the inflammation and lessens or resolves the pain.
- Diagnostic epidural spinal injections can be done at a very specific, isolated nerve to determine if that particular nerve is the source of pain. Sometimes only an anesthetic is injected. The immediate response to the injection is closely monitored. If the pain is completely or nearly completely relieved, then that specific nerve is the primary cause of the pain symptoms. If there is little pain relief, another source of pain exists.
Facet Joint Injection
Facet joint injections can also be done for both diagnostic and therapeutic reasons.
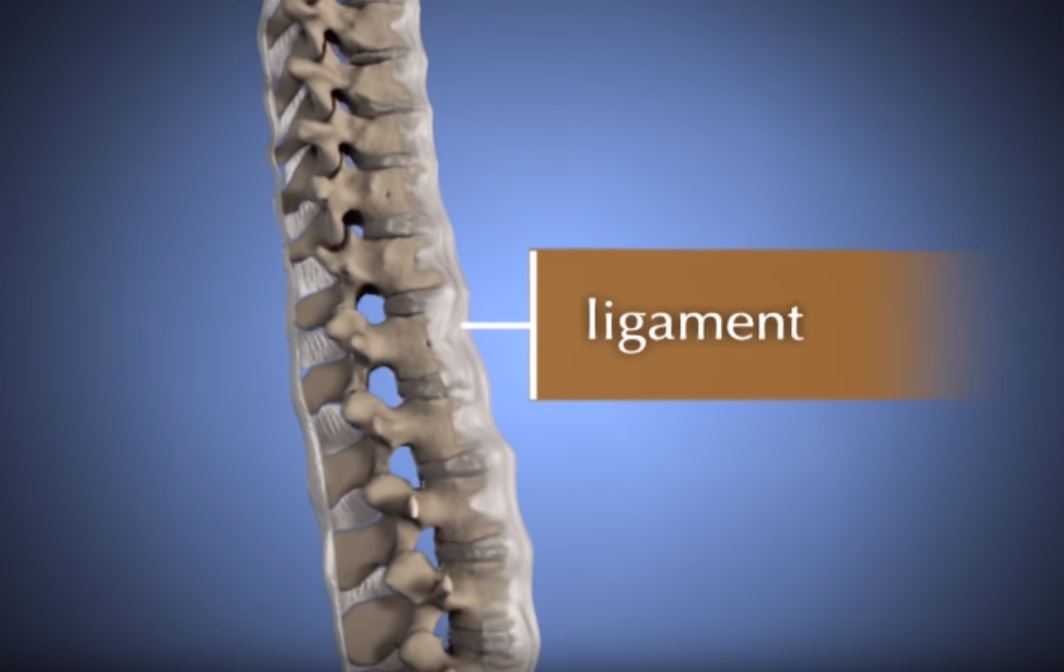
These types of injections are placed into and around the facet joints, which are the small joints located between each vertebra on the back of the spine. Facet joint injections are often used when pain is caused by degenerative/arthritic conditions or injury. They are used to treat neck, middle back, or low back pain. The pain does not have to be exclusively limited to the midline spine, as these problems can cause pain to radiate into the shoulders, buttocks, or upper legs.
For diagnostic purposes, facet joints can be injected in two ways:
- Injecting anesthetic directly into the joint
- Anesthetizing the nerves carrying the pain signals away from the joint (medial branches of the nerve).
If the majority of pain is relieved with anesthetic into the joint, a therapeutic injection of a steroid may provide lasting neck or low back pain relief.
If anesthetic injections indicate that the nerve is the source of pain, the next step is to block the pain signals more permanently. This is done with radiofrequency ablation, or damaging the nerves that supply the joint with a burning technique. The nerve that is burned is a sensory nerve that regenerates, so the effect of this treatment usually lasts several months.
Sacroiliac Joint Injection
Sacroiliac joint (SI joint) injections are similar to facet joint injections in many ways. The SI joints are located between the sacrum and ilium (pelvic) bones.
Problems in the SI joints have been shown to cause pain in the low back, buttock, and leg. Typically, one joint is painful and causes pain on one side of the lower body. It is less common for both SI joints to be painful at the same time.
This joint can also be injected for both diagnostic and therapeutic purposes.
- Anesthetizing the SI joint by injection under X-ray guidance is considered the gold standard for diagnosing SI joint pain. A diagnostic injection of the sacroiliac joint with anesthetic should markedly diminish the amount of pain in a specific location of the low back, buttock, or upper leg.
- A therapeutic injection will typically include a steroid medication, with the goal of providing longer pain relief.
Trigger Point Injection
Another type of injection is called a trigger point injection. Common conditions treated with trigger point injections include fibromyalgia, tension headache, and myofascial pain syndrome.
Similar to epidural and facet joint injections, trigger point injections involve injecting a combination of local anesthetic and, typically, an anti-inflammatory (such as a steroid) into the problem area. Trigger point injections can usually be done without X-ray guidance.
A similar technique called dry needling, in which a needle without medication is inserted into the trigger point, can be performed in a physical therapy office.
Provocation Discography
Provocation discography (also called discography or discogram) is a type of spine injection done only for diagnosis of pain. It does not have any pain-relieving effect. In fact, the goal is to try to reproduce a person's exact or typical pain to identify the source of longstanding back pain that has not improved with comprehensive, conservative treatment. This type of injection can severely aggravate the existing back pain.
Discography is performed much less commonly than the other types of spinal injections reviewed above. It is often used only if surgical treatment of low back pain is being considered. The information gained from discography can assist in planning the surgery.
- Discography involves stimulating and pressurizing an intervertebral disk by injecting a liquid into the jelly-like center (nucleus pulposus) of the disk.
- More than one disk is injected to distinguish a problem disk from one without symptoms.
- Criteria are used to identify a painful disk by provocation discography, including the type and location of pain and the appearance of the disk on an X-ray or computed tomography (CT) scan after the procedure.
Complications
Spinal injection procedures are generally safe procedures. If complications occur, they are usually mild and self-limited. The risks of spinal injections include, but are not limited to:
- Bleeding
- Infection
- Nerve injury
- Arachnoiditis (a pain disorder caused by inflammation of the arachnoid, one of the membranes surrounding the nerves of the spinal cord)
- Paralysis
- Avascular necrosis (death of bone tissue due to a temporary or permanent loss of blood supply; this rarely occurs in the spine)
- Spinal headache
- Muscle weakness
- Increased pain
Common side effects from steroids include:
- Facial flushing
- Increased appetite
- Menstrual irregularities
- Nausea
- Diarrhea
- Increased blood sugar, which is usually temporary
Some people are not good candidates for spinal injections. These include people with:
- Skin infection at the site of needle puncture
- Bleeding disorder or anticoagulation
- Uncontrolled high blood pressure or diabetes
- Allergy to contrast, anesthetics, or steroids
Last Reviewed
February 2022
Contributed and/or Updated by
AAOS does not endorse any treatments, procedures, products, or physicians referenced herein. This information is provided as an educational service and is not intended to serve as medical advice. Anyone seeking specific orthopaedic advice or assistance should consult his or her orthopaedic surgeon, or locate one in your area through the AAOS Find an Orthopaedist program on this website.